Technological advancements in medical imaging have enabled non-invasive diagnostics, establishing imaging as a critical component of healthcare systems. Medical image processing, an interdisciplinary field, is central to these advancements, involving processes from raw data acquisition to digital image transmission.
Modern imaging systems offer higher resolution in spatial and intensity dimensions and faster acquisition times, generating large volumes of high-quality raw data. Accurate processing and interpretation of this data are essential for reliable diagnostic outcomes. This article explores the core areas of medical image processing, specific imaging modalities, and key challenges and trends.
Core Areas of Medical Image Processing
Medical image processing encompasses three primary processes: image formation, image computation, and image management. These processes address distinct aspects of the imaging pipeline.
Image Formation
Data Acquisition
The initial step in image formation is acquiring raw imaging data, which contains information about physical quantities describing internal organs. Different imaging modalities rely on distinct physical principles. For example, digital radiography (DR) and computed tomography (CT) measure incident photon energy, positron emission tomography (PET) captures photon energy and detection timing, magnetic resonance imaging (MRI) processes radio-frequency signals from excited atoms, and ultrasound evaluates echo parameters.
The data acquisition process involves detecting physical quantities, converting them to electrical signals, preconditioning the signals, and digitizing the data. These steps are common across most medical imaging modalities.
Image Reconstruction
Image reconstruction is a mathematical process that forms images from raw data, often combining multiple datasets captured at different angles or time steps for multidimensional imaging. This process addresses inverse problems, a fundamental challenge in medical imaging. Reconstruction algorithms are categorized as analytical or iterative.
Analytical methods, such as filtered back projection (FBP) for tomography, Fourier transform (FT) for MRI, and delay-and-sum (DAS) beamforming for ultrasound, are computationally efficient. However, they rely on idealized models and struggle with complex factors like measurement noise or system physics.
Iterative algorithms overcome these limitations, improving noise robustness and reconstructing optimal images from incomplete data. These methods use system and statistical noise models, iteratively refining projections to minimize the difference between estimated and true values. Common iterative techniques include maximum likelihood expectation maximization (MLEM), maximum a posteriori (MAP), and algebraic reconstruction (ARC).
Image Computation
Image computation involves mathematical methods to enhance, analyze, and visualize reconstructed imaging data, extracting clinically relevant information.
Enhancement
Image enhancement improves the interpretability of image data through transformations. Spatial domain techniques, such as logarithmic, histogram, or power-law transforms, optimize contrast by directly manipulating pixels. Frequency domain methods, using frequency transforms, apply filters for smoothing or sharpening, reducing noise, improving contrast, enhancing edges, and eliminating artifacts.
Analysis
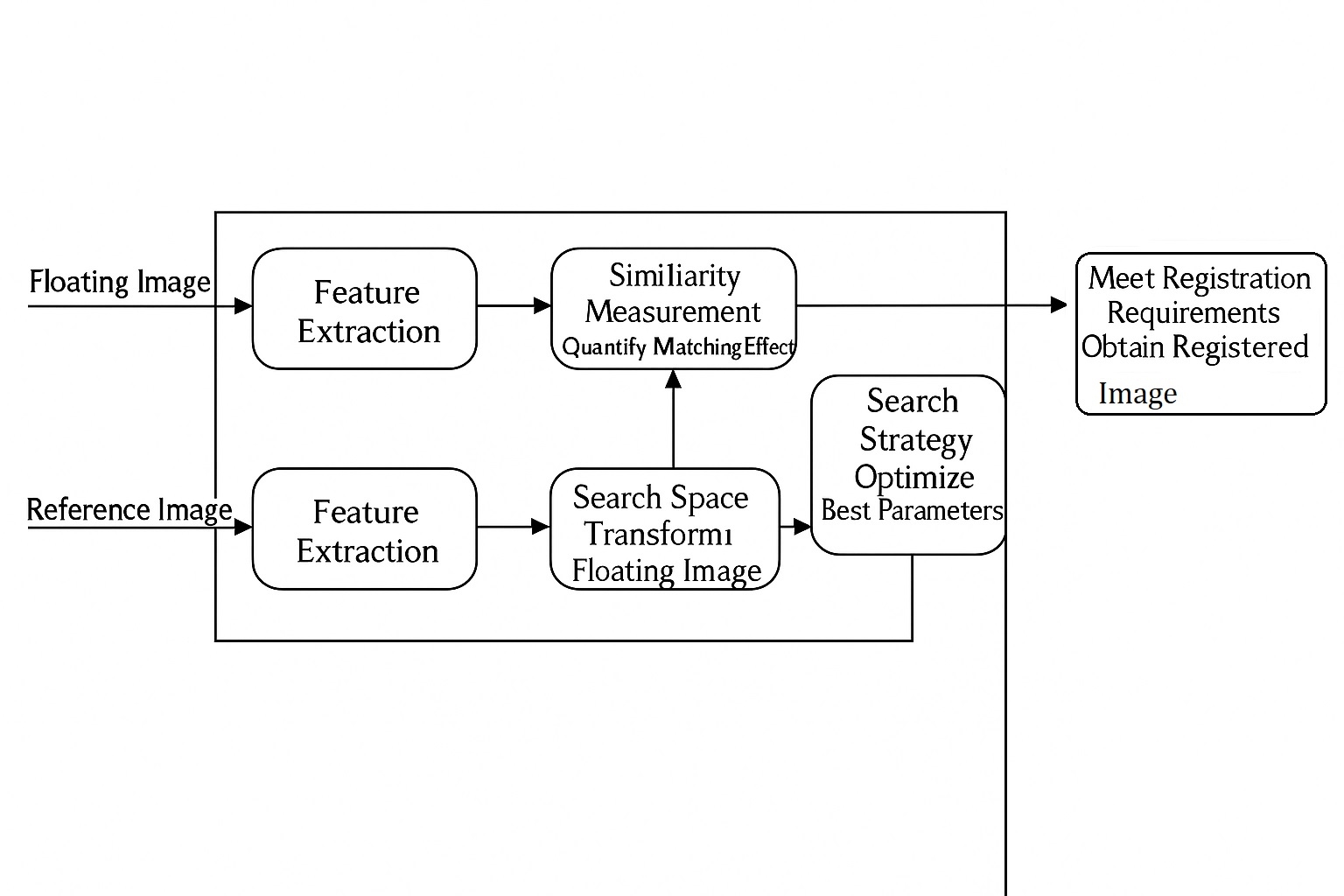
Image analysis includes segmentation, registration, and quantification. Segmentation divides images into meaningful anatomical contours. Registration aligns multiple images, critical for analyzing temporal changes or combining data from different modalities. Quantification determines properties like volume, diameter, or composition, directly impacting diagnostic accuracy.
Visualization
Visualization presents image data in intuitive formats, supporting analysis at initial, intermediate, and final stages. It aids processes like segmentation and registration and displays optimized results.
Image Management
Image management handles storage, retrieval, and transmission of imaging data. Standards like Picture Archiving and Communication Systems (PACS) enable efficient storage and access, while Digital Imaging and Communications in Medicine (DICOM) facilitates data storage and transfer. Specialized compression and streaming techniques optimize these tasks.
Challenges and Trends
Medical imaging is a conservative field, with research-to-clinical transitions often taking over a decade. Its complexity drives continuous innovation across its disciplines.
In data acquisition, advanced hardware improves data quality and information content, enabling faster scans, finer resolutions, and integrated modalities like ultrasound/mammography, CT/PET, or PET/MRI. Iterative algorithms are increasingly replacing analytical methods, enhancing PET image quality, reducing CT radiation doses, and enabling compressed sensing in MRI. Data-driven signal models and optimized algorithms address inverse problems more effectively.
As imaging systems generate more data and algorithms grow more complex, efficient computation is critical. High-performance graphics processors and multiprocessing technologies address this challenge, accelerating the transition from research to application.
Trends in image computation and management include advanced algorithms and standards, narrowing the gap between research and clinical practice. These developments enhance integration with physician workflows, improving the accuracy and reliability of imaging outcomes.
 ALLPCB
ALLPCB