Hypertension, a major risk factor for cardiovascular diseases, affects 1.28 billion people aged 30-79 globally, with nearly half unaware of their condition. Continuous blood pressure monitoring is critical for early detection and prevention, driving demand for wearable devices suitable for daily use.
Limitations of Traditional Methods
Blood pressure, the force of circulating blood against vessel walls, is traditionally measured using manual auscultation or oscillometric techniques in clinical or home settings. These methods are valuable but prone to inaccuracies due to operator skill, the "white coat" effect, and blood pressure variability. Ambulatory monitors, worn on belts or in pockets, use oscillometric cuffs to take readings every 15-30 minutes. While effective for assessing average blood pressure and diurnal patterns, they cannot provide continuous data, limiting insight into dynamic responses during daily activities.
Continuous Monitoring Techniques
Continuous blood pressure monitoring has gained attention, with techniques like volume clamping and tonometry being common. However, these methods require constant skin pressure, causing discomfort, and are sensitive to motion artifacts or require frequent calibration. Alternative approaches include:
- Pulse Transit Time (PTT): Measures the time for a pressure wave to travel between two arterial sites. PTT shortens with higher blood pressure due to increased vascular tension.
- Pulse Arrival Time (PAT): Uses electrocardiogram signals as a proximal waveform reference, similar to PTT.
- Pulse Wave Velocity (PWV): Calculated as PWV = L/PTT, where L is the distance between proximal and distal sites, reflecting arterial stiffness.
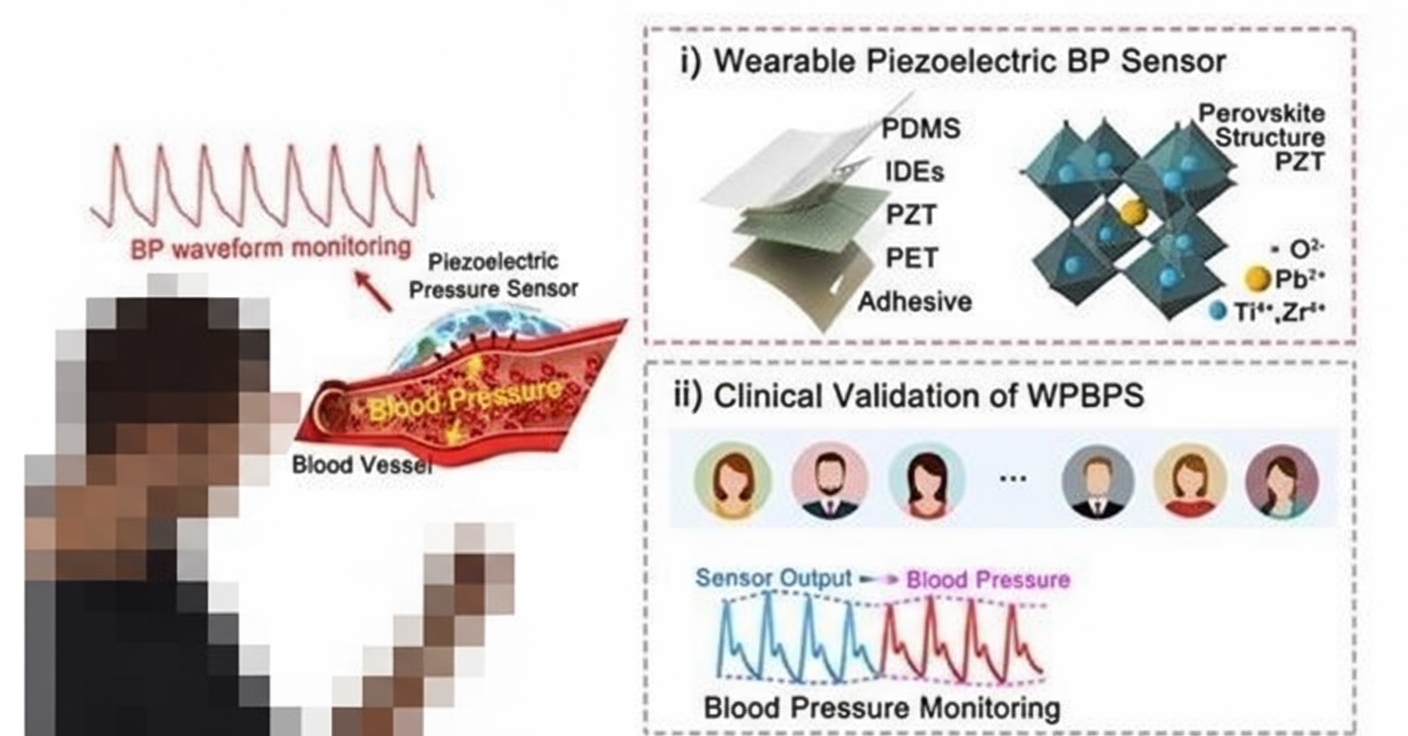
- Pulse Wave Analysis (PWA): Extracts features from arterial waveforms, requiring only a single sensor, and can be combined with PTT for improved accuracy.
- Facial Video and Ultrasound Methods: Extract arterial waveforms or vessel diameter changes, but require cuff-based calibration.
These methods, often data-driven and enhanced by machine learning, struggle with generalization across individuals and require subject-specific calibration. Few meet the AAMI standard (mean error < ¡À5 mmHg, standard deviation < 8 mmHg) for universal use without calibration.
Innovative Wearable Solution
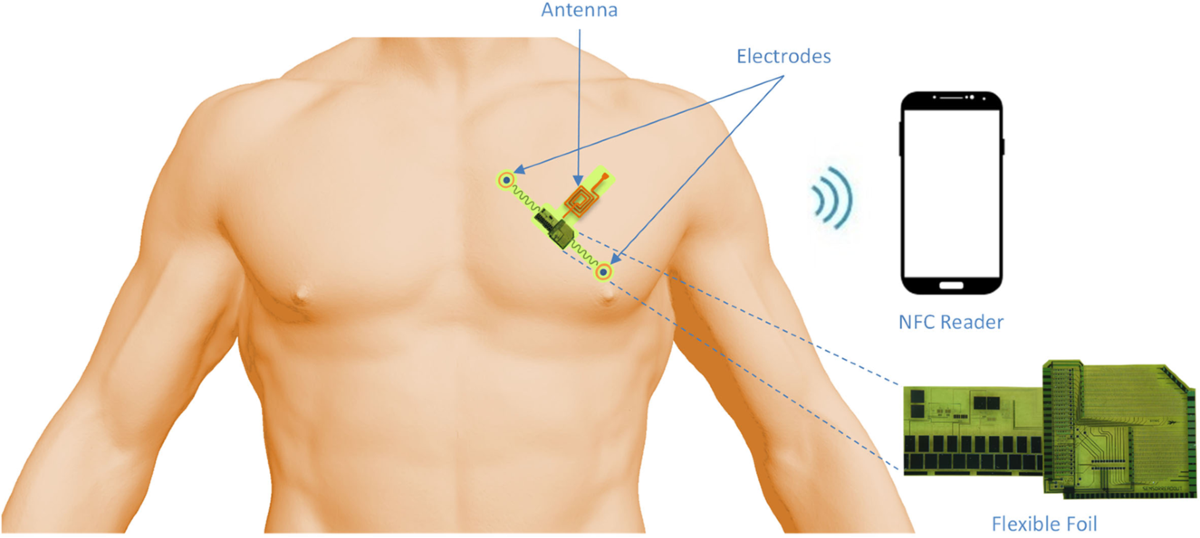
A research team from Tsinghua University¡¯s Department of Precision Instruments developed a smartwatch for non-invasive, continuous blood pressure monitoring. The device uses dual photoplethysmography (PPG) sensors on both sides of the wrist to capture cardiac output and pulse waveform features, alongside an interface sensor for contact pressure and skin temperature. Machine learning algorithms fuse these multi-channel signals to estimate blood pressure in real time.
The dual PPG setup mitigates individual and wear-related signal variations, improving universality. Contact pressure and skin temperature data further enhance measurement consistency. Compared to existing methods, this approach offers higher accuracy and better generalization, requiring no subject-specific calibration. Its simple design and low computational load make it a practical solution for early detection of health deterioration.
Future Improvements
Ongoing research aims to enhance the device by:
- Optimizing sensor design for better skin contact and reduced environmental interference.
- Refining data fusion algorithms to improve diastolic blood pressure estimation.
- Adapting the system for specific scenarios, such as motion or sweating.
This wearable technology advances continuous blood pressure monitoring, offering a scalable solution for global healthcare applications.
 ALLPCB
ALLPCB