Overview
Breath analysis was first performed by chromatography in the 1970s, demonstrating organic compounds in exhaled air. Since then, more than 3,000 volatile organic compounds (VOCs) have been identified in breath and investigated for potential medical applications. Aside from breath alcohol detectors, few sensor devices have reached high technological maturity, and diagnostic use has largely remained confined to chromatographic laboratory testing. Advances in materials science, synthetic biology, and engineering, together with renewed interest in diagnosing infectious disease from exhaled breath, have recently accelerated attention to breath analysis.
According to Mems Consulting, researchers at the University of Freiburg recently published a review titled "Wearable breath analysis" in Nature Reviews Bioengineering, outlining milestones and challenges for wearable devices applied to breath analysis in clinical contexts.
Breath Analysis as a Diagnostic Tool
Breath analysis can be broadly understood as a two-step process: validating diagnostic breath biomarkers and establishing methods to detect them. Specific VOCs associated with certain diseases or metabolic activities have been identified in clinical trials as so-called "breath prints." As a result, breath analysis can serve as a noninvasive qualitative diagnostic tool. Compared with other noninvasive sampling methods, breath sampling has a unique advantage because analytes transfer from blood to the lung while bypassing complex transport mechanisms.
Wearable Breath Sensors
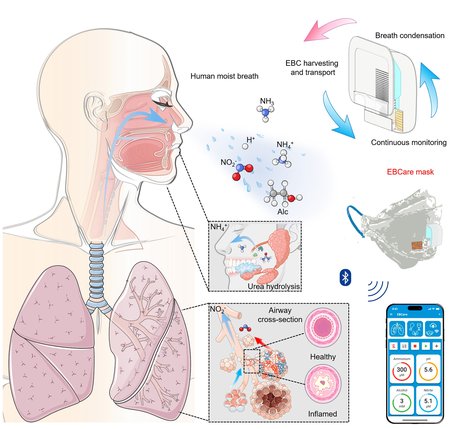
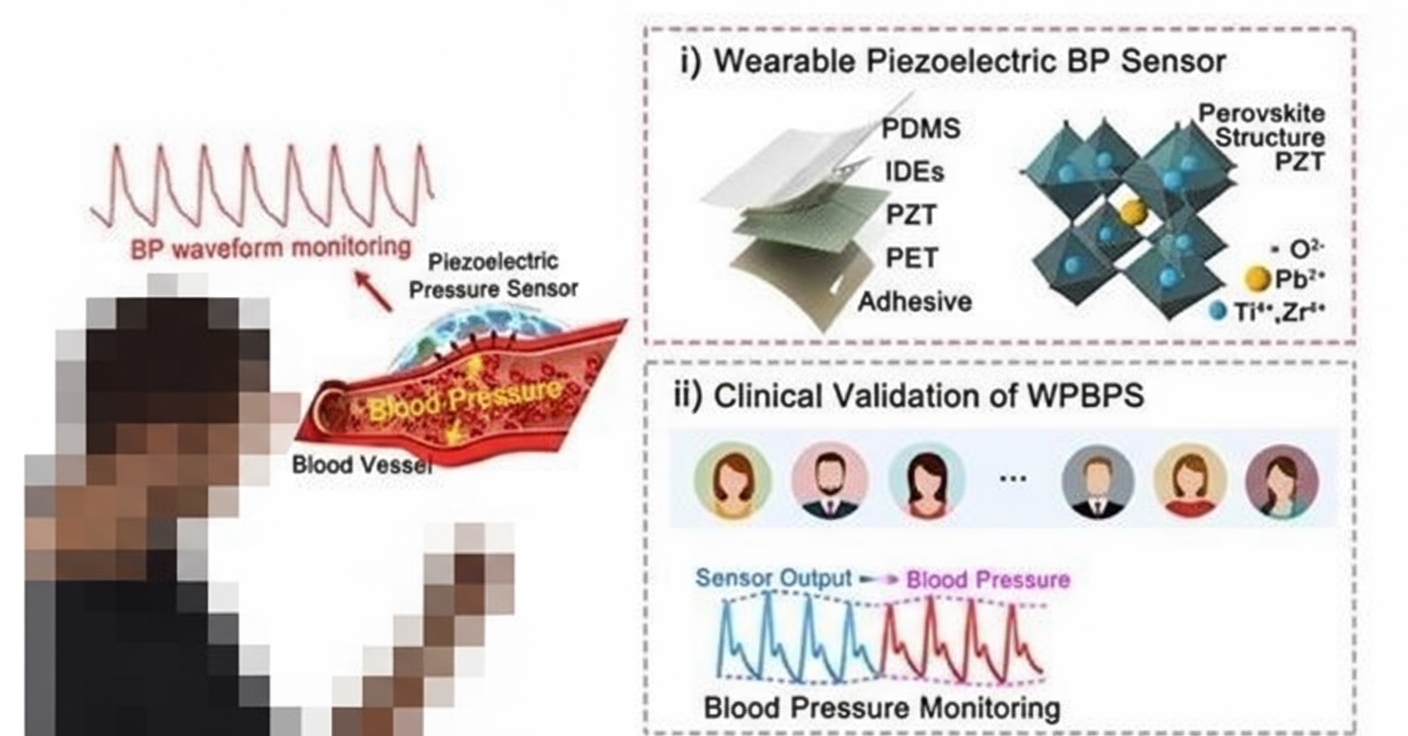
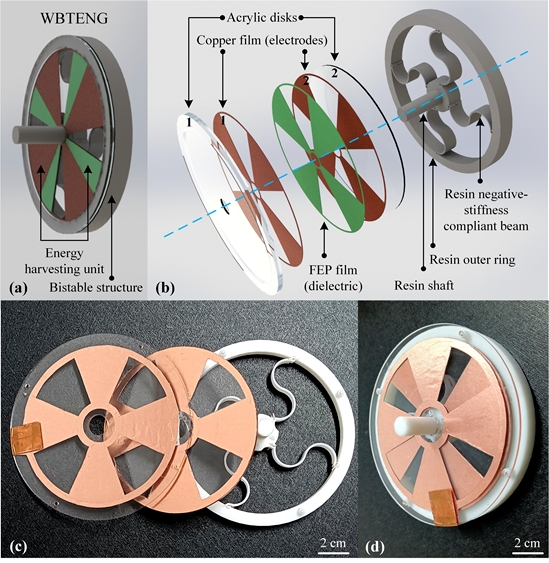
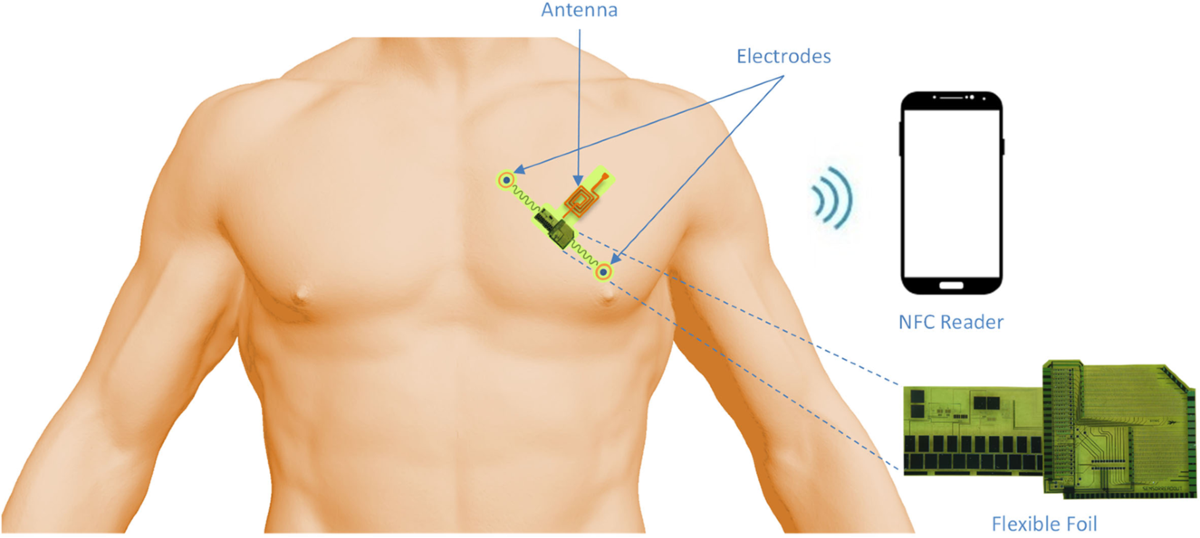
Transitioning from laboratory-based measurement techniques to wearable biosensors is necessary to accelerate the translation of breath analysis. Mask-form wearables can detect hydrogen peroxide, a biomarker for several respiratory conditions such as asthma, chronic obstructive pulmonary disease, and cancer, using electrochemical sensing, and they can monitor respiratory patterns (respiratory rate, coughing, breath-holding) via integrated self-powered pressure sensors. The COVID-19 pandemic further promoted breath analysis at the point of care as a means to detect airborne transmission from virus-containing aerosols. For example, masks with freeze-dried CRISPR-based sensors can detect SARS-CoV-2 nucleic acid using lateral-flow formats; optical "sniffers" (colorimetric sensor arrays) can semi-quantitatively assess COVID-19 severity by correlating color patterns with clinical reports and RT-PCR results.
Several challenges must be addressed to realize the clinical potential of wearable breath analysis.
Sensitivity
Although many breath analytes have been identified (roughly 3,500), including exogenous markers, their concentrations in breath are typically very low—often 1,000 to 10,000 times lower than in blood—varying with age, diet, smoking, medication, and exhalation flow rate. Therefore, wearable breath analyzers must achieve high sensitivity to detect target analytes. Concentration of target molecules is needed either at the wearable sensor or at the source (lung and/or airways).
In wearables, analytes can be separated and preconcentrated using microfluidic systems, such as micro-gas chromatography. Sensory elements can gain sensitivity through synthetic-biology-based bioassays (for example, CRISPR–Cas systems, microbial enzymes, and proteins) or by engineering nanostructures to increase effective sensing area. Target molecules can also be concentrated at the source by stimulating metabolic activity, or exogenous biomarkers can be expressed at the source by leveraging disease-associated metabolism or engineered living organisms. Chemical pretreatment or formation of analyte–nanoparticle conjugates can further enhance analyte reactivity.
Selectivity
Measuring a specific analyte within mixtures of substances with similar chemical or physical properties requires design strategies that address incompatibility. In top-down approaches, sensor arrays are used to improve selectivity. Each sensing unit must be robust and apply a range of chemical interactions to capture different combinations of informative compounds. Interpretation relies on measuring similarities or differences, so large datasets must be compiled and processed with pattern-extraction models to associate physiological states with sensor fingerprints.
However, the same subset of sensors can be activated by different analyte combinations, complicating the association of patterns with specific conditions. This dilemma can be mitigated by balancing complexity across sensing hardware and model architecture. Breath contains rich chemical diversity, and prior prediction of relevant analyte subsets remains challenging. Multi-array sensing technologies should therefore be sufficiently complex to respond to compositional changes. Olfactory receptors are the only known sensing units that reflect this complexity and could be integrated into hybrid biosensors in wearable devices. Data must be processed with similarly complex "black-box" models, such as deep learning methods, which require large training datasets.
Sampling
Breath composition is strongly influenced by sampling methodology, which is not standardized. Relative ratios of analytes vary with breath phase (for example, end-tidal), breathing pattern, sample contamination (such as saliva), sampling mode (online continuous versus offline discrete), and sample phase (vapor/gaseous versus condensate). Therefore, end-to-end wearable design should adopt a sampling strategy that supports continuous acquisition of physiological state. Disposable masks can integrate sampling, sample preparation (if needed), and sensing modules. Alternatives include subnasal or intranasal patches and implants in the airway (potentially self-powered by metabolites such as lactate or glucose). Nebulization modules integrated with sensors could enable closed-loop drug delivery for therapeutic applications.
Ethical Considerations
Ethical issues related to wearable breath analysis include patient data collection, safety, duty of care, legal liability, user compliance, accessibility, and fairness. These considerations must be addressed during device design and clinical deployment. Patient safety and duty of care are particularly important for therapeutic wearables. Legal liability arises from integrating patient data into data pipelines and from errors or bias in model and training database selection, which in turn affect the influence of wearable outputs on final diagnostic decisions. Device misuse and lack of software updates, given programming languages, databases, and disease-specific clinical cues, can also create liability issues.
Outlook
By addressing the technical and ethical challenges described above, wearable breath analysis has the potential to complement distributed preventive health monitoring and to change aspects of diagnostic practice.
 ALLPCB
ALLPCB